Stroke
Stroke is a medical emergency that occurs suddenly and can be life-threatening. As such, it is one of the leading causes of everyday disability and death in old age.
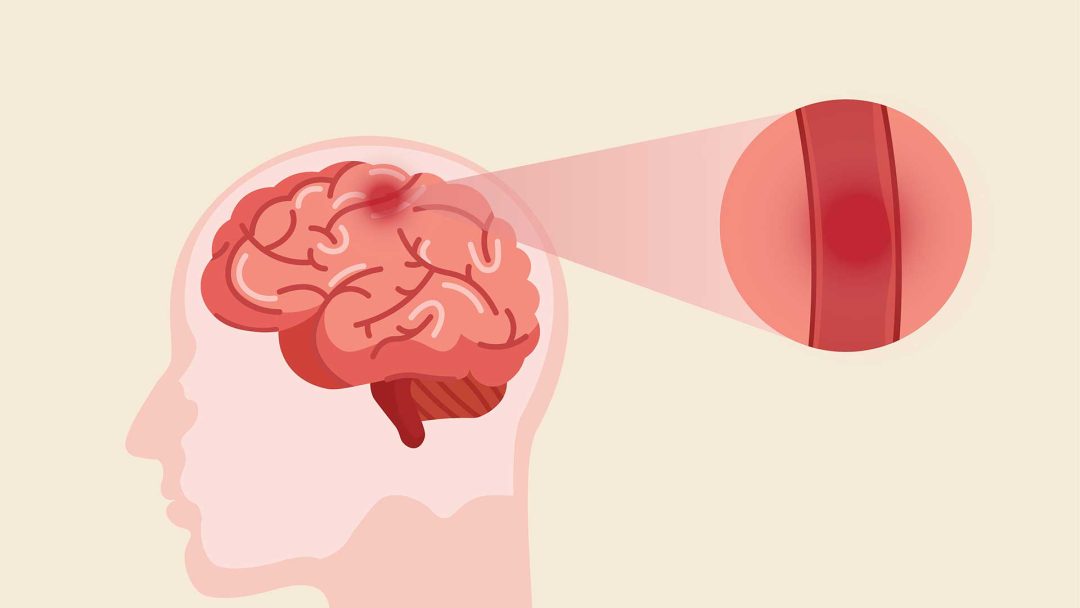
The cause is an undersupply of oxygen to the brain, which can lead to the affected tissue being permanently destroyed.
In the following article, we take a closer look at possible causes, symptoms, treatment options and prevention and provide answers to the most frequently asked questions about strokes.
What is a Stroke?
A stroke is a circulatory disorder of the brain that can lead to a number of functional deficits and, in the worst case, death. It is also known as a cerebral infarction, a cerebrovascular accident (CVA), a brain attack, or an apoplexy.
There are two main triggers in the development of a stroke.
The first is a sudden blockage or closing (occlusion) of the blood vessels. This acute vascular occlusion leads to an undersupply of oxygen (ischaemia) and ultimately to the death of the brain tissue.
This is to be distinguished from hemorrhagic stroke, in which the primary cause is a bleeding in the brain tissue. This is also called a cerebral haemorrhage, which leads to compression of important structures and ultimately to the death of the tissue. This can be triggered by a ruptured blood vessel due to a fall or accident, but also due to a burst aneurysm, which is a weak knot in the blood vessels.
In both cases, immediate action is required, as the brain tissue cannot survive long without oxygen supply and most areas of our brain fulfils vital tasks for physical and mental function.
Causes of a Stroke
The causes of a stroke are, as mentioned above, either a cerebral infarction or a cerebral haemorrhage. Both have different risk factors that should be taken into account.
Cerebral Infarction
A cerebral infarction, or ischaemic stroke, leads to reduced blood flow and supply to the brain. Ischaemia describes the acute undersupply of oxygen to the tissue. Due to its high energy consumption, the brain can only compensate for this reduced blood supply for a short period of time before the brain tissue dies off. Thus the damage can be quickly and permanently.
A cerebral infarction is triggered by small clots that cut off the arterial supply to the brain, resulting in a blockage of these blood vessels (acute vascular occlusion), and, depending on the vessel, contribute to characteristic failure patterns.
Risk factors for an ischaemic stroke include hypercholesterolemia, diabetes, smoking, lack of exercise, infectious diseases, hidden inflammation and gastrointestinal diseases. They can contribute to the formation of a blood clot (thrombus), which travels into small vessels and blocks the blood flow to certain areas of the brain.
Cerebral haemorrhage
A cerebral haemorrhage, or haemorrhagic stroke, is caused by bleeding in the head. This leads to important structures being squeezed, cut off from oxygen and dying as a result.
Cerebral haemorrhages are often the result of acute trauma to the head, for example a blow or a fall. However, a burst aneurysm can also lead to a cerebral haemorrhage.
Old age, arteriosclerosis, high blood pressure, alcohol abuse and an unhealthy lifestyle make the blood vessels less elastic, causing them to rupture more quickly, which results earlier in a cerebral haemorrhage.
Risk Factors for a Stroke
There are a number of risk factors that influence the likelihood of a stroke. One risk factor is genetic, meaning the presence of strokes in the family (positive family history).
However, the most important risk factors include arteriosclerosis, high blood pressure, diabetes, obesity and cardiovascular disease. Furthermore, factors such as intestinal health, hidden inflammation, chronic infectious diseases and metabolic disorders should also be taken into account.
All of these chronic diseases can be at least partially controlled through a balanced diet, regular exercise and should be a central part of a healthy lifestyle. Such a lifestyle change, in combination with appropriate therapies, can be done under supervision of an experienced integrative medical doctor.
Symptoms of a Stroke
The symptoms and consequences of a stroke vary drastically depending on the localisation of the stroke in the brain. The brain has three main parts: the cerebrum, cerebellum and brainstem, which all have different functions.
Depending on which part is affected, different symptoms arise. For example, speech and motor function may be impaired, and vital centres such as breathing may stop.
In general, a focal gaze (stare) of one eye can be the first sign of a stroke, as a result of the affected side of the brain. Moreover, double vision, flickering of the eyes or loss of vision may occur.
Below, we will discuss all these in detail.
Stroke in the Cerebrum
The cerebrum, the largest part of the brain, performs higher functions such as interpreting touch, emotions, vision and hearing, speech, reasoning, learning, and fine control of movement. Therefore, a stroke in the cerebrum, also known as a cerebral infarction, affects in most cases the execution of movements, sensory perceptions, emotions and speech. Those affected can also suffer memory loss and a change in behaviour.
With early detection and treatment as well as extensive rehabilitation measures, it may be possible to restore some of the function, as the plasticity of the neurons allows the areas to be reorganised.
Cerebellar Infarction
The cerebellum is clearly differentiated from cerebral infarction in terms of symptoms. The cerebellum, located under the cerebrum, coordinates muscle movements, balance and posture.
Therefore, a cerebellar infarction can lead to dizziness, balance problems, fine motor function disorders and uncontrolled eye movements. Rapid action is also required here in order to minimise long-term damage.
Brain Stem Infarction
The brainstem, a small region below the cerebrum, is alongside the cerebellum the most common site for strokes. The brainstem acts as a relay centre connecting the cerebrum and cerebellum to the spinal cord. Many automatic functions such as breathing, heartbeat, blood pressure and alertness are localised in the brain stem.
Due to the high density of these vital functions, brain stem infarctions can have serious consequences or even lead to death. Thus, these have a worse prognosis than infarctions in other areas of the brain and the chances of survival decrease drastically with every minute of inadequate treatment.
Thalamic Infarction
The thalamus is an important structure in the brainstem that supports the processing of sensations, the regulation of the sleep-wake cycle and the control of consciousness and attention.
If a thalamic infarction occurs, a very diffuse symptom picture can develop, including clouding of consciousness, sensory perception disorders, but also defects in speech comprehension. Orientation in space can also be impaired, which is known as pusher syndrome.
The thalamus is only affected in around 3% of cases. Fortunately, it has a better prognosis than other brainstem infarctions.
Stroke in the Eye
As the retina of the eye is part of the central nervous system, a reduced blood supply here is also referred to as a stroke. A stroke in the eye can lead to retinal vein occlusion as well as retinal artery occlusion. They differ slightly in their symptoms, but both have an acute loss of vision in common.
This sudden loss of vision in one eye, also called “amaurosis fugax”, is painless and of short duration. However, it can lead to permanent blindness if left untreated.
If you notice sudden changes in vision, which may be accompanied by headaches, dizziness, weakness and speech difficulties, you should seek medical treatment immediately to avoid permanent vision loss.
What are the Signs or Early Warning Signs of a Stroke?
It is important to recognise the signs or early warning signs of a stroke in yourself or others, as early recognition and prompt action will significantly improve treatment and outcome.
- Numbness and tingling, often limited to one side of the body
- Speech impairment or difficulties in understanding speech
- Sudden visual disturbances
- Balance problems and coordination disorders
- Severe, sudden headaches
Silent Stroke
A silent stroke, also called an asymptomatic cerebral infarction, is a stroke that does not manifest itself through consciously recognisable symptoms. It is therefore much more likely to go unrecognised, but can lead to just as much long-term damage as a stroke with clearly recognisable symptoms.
Even the smallest changes in motor function, speech or even personality can be an indication of a stroke and must be taken seriously. The only way to diagnose a silent stroke is with a brain CT scan or anMRI.
The top priority should be to restore blood flow quickly and prevent a recurrence in the future, which could potentially cause serious damage.
TIA - Transient Ischaemic Attack
A Transient Ischaemic Attack (TIA), also known as a mini-stroke, occurs when the blood supply to a part of the brain is temporarily interrupted.
However, unlike a classic stroke, a TIA does not cause permanent brain damage and the symptoms usually disappear within minutes to hours without leaving permanent damage.
The symptoms are similar to those of a stroke, but are usually not as severe.
Even if the symptoms subside after a short time, a TIA should be taken seriously, as patients with TIA have a higher risk of having a stroke. The risk factors should be checked and treated if necessary.
Stroke Test
There are a number of brief tests that can assist in recognising a stroke. A very common scheme is the FAST rule. This involves taking a closer look at the face, arms, speech and time to call for help as quickly as possible. See below for more details.
Nevertheless, it is not said that if the tests are all negative, there cannot be a stroke. A doctor should be consulted if there are any unusual sensations to rule out a stroke.
Fast Test for Stroke
The Fast Test is a reminder of important clues for rapid stroke recognition.
Face
The F stands for face and is intended to remind that changes in facial expressions are often noticeable during a stroke. The eyelid, cheek, or corner of the mouth can droop on one or two sides or the tongue can no longer be properly controlled. Ask the other person to smile and pay attention to both corners of the mouth. Are there any differences?
Arms
A stands for arms and tests motor skills. Ask the person to stretch both arms out in front of their body and see if one arm drops.
Speech
The letter S stands for speech. Speak a sentence and ask the other person to repeat it. Are there any difficulties with pronunciation or speed?
Time
If one or more of these tests are positive, you need to act quickly, because every minute counts after a stroke. This is what the T with the time stands for.
Tongue Stroke Test
If a stroke is suspected, a look at the tongue can confirm the suspicion.
If it deviates to one side or curves, this may be a sign of a stroke.
Nevertheless, even if the tongue test is negative, a doctor should be consulted if other symptoms persist.
NIHss Score
The National Institutes of Health Stroke Scale (NIHss) is a tool used by healthcare professionals to assess the severity of a stroke. It provides a standardised assessment of the patient’s neurological function and is often used for both diagnosis and progression.
It is made up of factors such as consciousness, field of vision, strength, limb sensitivity, speech and attention. In all categories, points can be awarded from 0 for normal to 6 for severely impaired in order to obtain an overall assessment of the patient.
Consequences of a Stroke
How severe and restrictive the consequences of a stroke can be depends largely on the area of the brain affected and the time between the infarction and treatment.
If action is taken quickly, symptoms can normalise completely. However, permanent signs of paralysis, loss of vision, speech problems or death can also occur.
Immediately after a stroke, it is usually difficult to predict how well the patient will recover during rehabilitation.
Treatment of Stroke
A stroke is a medical emergency and must be treated immediately.
Ischaemic strokes are treated by removing the thrombus (blood clot). The thrombus is removed by dissolving it with medication (known as lysis therapy) or by mechanical removal using a catheter (thrombectomy).
In haemorrhagic strokes, the location and cause of the bleeding must first be determined in order to drain the blood, reduce the pressure on the brain and then stop the bleeding.
In general, the faster a patient is treated, the better the chances of recovery.
Stroke Unit - Stroke Ward
The stroke unit is a ward that specialises in the treatment of infarcts.
As a stroke unit, it is prepared to provide fast, high-quality treatment at all times in order to offer the patient the best possible treatment outcome.
It consists of a multidisciplinary team of doctors, nurses, physiotherapists, occupational therapists and speech therapists, so that rehabilitation measures can begin immediately after treatment and the patient’s individual needs can be optimally catered for.
REHA - Rehabilitation
Rehabilitation is a central component of stroke care and is indispensable when it comes to regaining everyday function and quality of life. It begins immediately after treatment so that no valuable time is lost.
Rehabilitation measures are usually carried out by an interdisciplinary team consisting of doctors, physiotherapists, occupational therapists, speech therapists, neuropsychologists, social workers and other specialists.
Depending on the loss of function, wishes and needs of the patient, rehabilitation can focus on different areas in order to restore their ability to perform everyday activities.
In addition, rehabilitation can help to educate, support and accompany the family and relatives with the current situation.
How can a Stroke be Prevented?
Preventing a stroke requires a healthy lifestyle, control of risk factors and regular medical screening at an early stage.
Preventive measures include a balanced diet with high-quality fats, regular exercise and avoiding high blood pressure.
The following aspects are also important for the prevention of stroke:
- Control of the intestinal flora
- Control of chronic infectious diseases such as Lyme disease or EBV
- Control of hidden inflammations, such as jaw inflammation, periodontitis or chronic inflammatory bowel disease
- Control of hidden micronutrient deficiencies, for example in HPU
- Control of toxin exposure
- Control of hidden intolerances and immune disorders
These factors can negatively affect the vascular walls and increase the risk of arteriosclerosis and stroke. Therefore, proper treatment is recommended to prevent strokes.
In order to be able to make an up-to-date risk assessment, it is worth having an examination by your doctor. If necessary, other risk factors can be recognised and treated to reduce the likelihood of a stroke.
Average Life Expectancy After a Stroke
The average life expectancy after a stroke depends on various factors. These include, for example, the severity of the stroke, the effectiveness of treatment and rehabilitation, the prevention of secondary diseases and the individual health of the patient.
The survival rate five years after a stroke is 55%, but varies greatly between the different age groups.
It is therefore particularly important to take the event seriously, make lifestyle adjustments and eliminate risk factors in order to prevent another stroke and to enjoy a long and healthy life.
First Aid in the Event of a Stroke
First aid measures in the event of a stroke can be crucial when it comes to minimising long-term damage. There are guidelines which you can follow until professional help arrives.
The first and most important step is to inform the emergency doctor and make a note of the time of onset of the stroke, as this may be important for treatment later on.
Next, the affected person should be placed in a supine position with their upper body slightly elevated to facilitate breathing. In addition, the patient can be reassured to alleviate anxiety.
Fluids, food or medication should not be administered unless it is specifically requested from the medical staff.
If the patient becomes acutely unwell and the heartbeat stops, a heart rhythm massage must be started.
Follow these measures until help arrives to improve the chances of recovery.
Med. pract. Dana Hreus M.A.
A stroke has many aspects that should be taken into account. An individualised diagnosis and elimination of the causative factors can significantly support the body and prevent future strokes.

Frequently Asked Questions and Answers on the Subject of Strokes
Stroke is an extremely complex condition that raises many questions and can be very intimidating. Below you will find the most frequently asked questions and answers about symptoms, treatment and prognosis.
If you have any further questions, please do not hesitate to ask your doctor.
An insidious stroke may not be recognised immediately as the symptoms are often subtle and mistaken for signs of ageing.
These include mild cognitive decline and slowness, behavioural changes, mild speech disorders or motor difficulties.
If you notice these changes in yourself or others, it is advisable to seek medical advice so that a stroke is not overlooked.
It may be a stroke, especially if it is accompanied by motor symptoms, numbness or speech difficulties.
In any case, it is worth seeking medical clarification if you have not experienced this sensation before and if the cause is unknown.
If the tingling sensation is accompanied by other stroke symptoms, you should seek clarification. Otherwise, tingling in the lip is not a classic symptom of a stroke.
Blood in the eye is not a classic symptom of a stroke, but should nevertheless be examined by a doctor immediately, especially if it is accompanied by pain and loss of vision.
How long a stroke is detectable depends on the type, severity and means of diagnosis.
MRI can sometimes be used to recognise infarcts that occurred years ago and even draw rough conclusions about when the stroke occurred.
Yes, strokes can vary greatly in their severity, both spatially and in the extent of the functions affected.
The mildest form is the transient ischaemic attack (TIA), in which a temporary lack of blood supply to an area can lead to classic stroke symptoms. However, it subsides completely on its own within minutes to hours.
Although stress is not considered a direct trigger for a stroke, it is an important risk factor for many health conditions and often leads to an unhealthy lifestyle.
The aim should be to recognise stress and find a healthy way of dealing with stressors that cannot be avoided.
The emergency doctor should be alerted, the person should be placed in a supine position with the upper body slightly elevated and the person should be reassured.
In the event of cardiac arrest, cardiac rhythm massage must be initiated.
A mild stroke can cause sudden weakness, visual disturbances, slight changes in speech, numbness and motor disorders.
However, the symptoms are often very mild and can only be recognised on closer inspection.
Symptoms of a severe stroke can include hemiplegia, severe headaches, speech impairment, altered facial expressions, loss of consciousness and loss of vision.
If these symptoms occur, immediate action must be taken and treatment started.
The left side of the brain is responsible for speech and the motor functions of the right side of the body. Consequently, a left-sided stroke leads to right-sided paralysis, speech and comprehension disorders.
Another symptom can be hemianopsia, where the affected person is no longer able to correctly recognise objects in the right field of vision.
Exactly which functions are affected depends on the individual case and must be determined by detailed tests.
The right hemisphere of the brain is responsible for spatial orientation and the motor functions of the left side of the body. Consequently, a right-sided stroke leads to left-sided paralysis and orientation disorders.
Another symptom can be hemianopsia, where the affected person is no longer able to correctly recognise objects in the left field of vision.
The time to death after a stroke varies greatly and depends on several factors, including the severity and type of stroke, the areas of the brain affected, timely medical care and the health of the person before the stroke.
A stroke can lead directly to death or can be successfully treated and not stand in the way of continued life.
No, tinnitus is not a classic warning sign of a stroke.
However, if it occurs in combination with other neurological symptoms, it should be investigated.
The prognosis for a cerebral haemorrhage varies considerably depending on the location of the haemorrhage and the time until it is discovered.
If the haemorrhage is small and is detected quickly, a full recovery is possible.
The likelihood of a stroke increases with age. The incidence is particularly high from the age of 65.
A heart attack is characterised by the classic triad of symptoms of chest tightness, accompanied by cold sweats and radiating pain in the left arm.
A stroke is characterised by paralysis, speech impairment and headaches.
It can be difficult to distinguish between a migraine and a stroke, as some symptoms overlap.
However, sudden onset of weakness, numbness and signs of paralysis are typical of a stroke.
If you are unsure, you should visit the doctor to have the cause clarified.
A stroke can affect life expectancy, although the effects depend on various factors. These include the severity of the stroke, timely medical care, the effectiveness of rehabilitation and the treatment of risk factors for future strokes and cardiovascular disease.
In principle, driving is possible again after successful rehabilitation, but your ability to drive must be checked again before you are allowed to drive again.
If permanent damage from the stroke remains, the car may have to be adapted to your own limitations.
Resilience after a stroke depends largely on the severity of the stroke, your health and the quality of your rehabilitation.
In principle, full resilience is possible again, although permanent restrictions may remain.
After a stroke, blood values such as inflammation markers, coagulation factors, electrolytes and, in the case of haemorrhage, the number of blood cells can change.
In the course of treatment, these changes are addressed and treated accordingly so that they return to a physiological range.
Blood thinners are a widespread and effective way of making a recurrence less likely.
However, a healthy lifestyle and the treatment of underlying diseases are also crucial when it comes to staying healthy in the long term.
Talk to an experienced doctor about the causes of strokes and how to prevent them from reoccuring.
The second stroke does not necessarily have to be fatal, but it usually has more severe consequences than the first stroke.
Yes, strokes increase the risk of vascular dementia. It is therefore important to reduce risk factors as far as possible and to adhere to long-term treatment strategies.
No, there is no evidence that neck cracking can lead to strokes.
Saccadic training after a stroke can help compensate for visual difficulties by performing targeted exercises to improve the accuracy, speed and coordination of eye movements.
A cryptogenic stroke is a stroke without a clearly recognisable cause.
Further information
The information listed contains relevant topics and serves to improve understanding.