Stool Examination
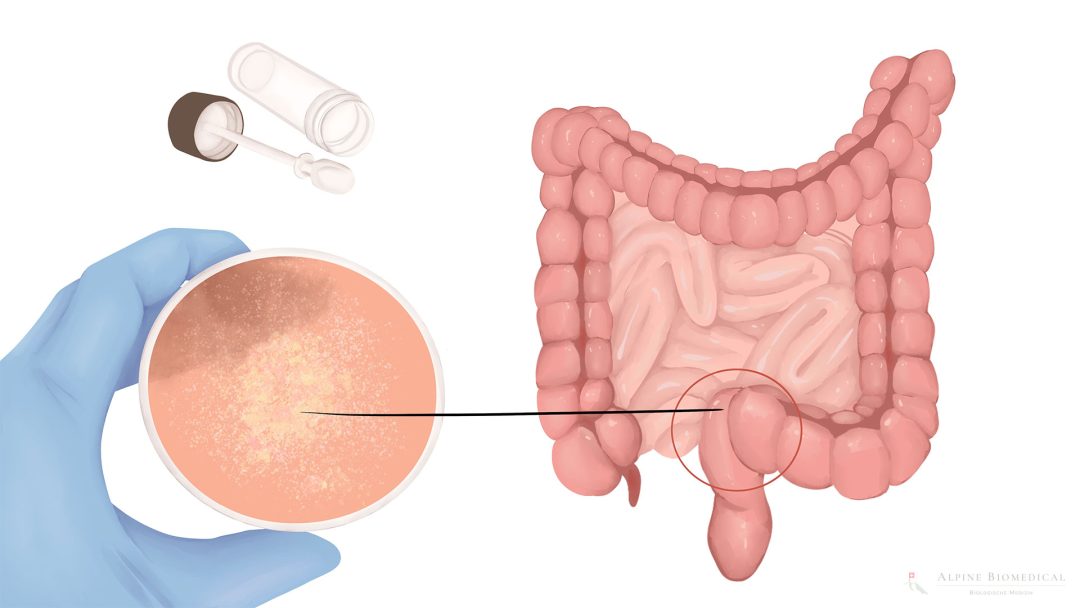
A stool examination is a test that is often ordered by doctors, where a sample of the patient’s stool is analysed in a laboratory. This type of laboratory diagnosis expands the possibilities of patient diagnosis and gives information on various physical parameters.
The stool examination provides information about the intestinal flora (microbiome of the intestine) whereby possible unhealthy colonisation or microbial compositions are listed. As the intestine plays a key role in the immune system and detoxification, a precise breakdown of the microbes, yeasts and parasites is of great importance in the treatment of various diseases.
Digestive enzymes and undigested food components or digestive residues can also be detected during the stool examination and further conclusions can be drawn about the effectiveness of a patient’s digestion.
The physician can also obtain indications of intestinal inflammation, leaky gut or food intolerances.
Special tumour markers in the stool can also support the diagnosis of cancer or precancerous lesions.
Med. pract. Dana Hreus M.A.
When ordering and evaluating stool tests, the doctor's experience is an important basic requirement in order to avoid misinterpretation of the laboratory results.

Further information
Further information intended to give a better overview of the topic.