Testicular Cancer
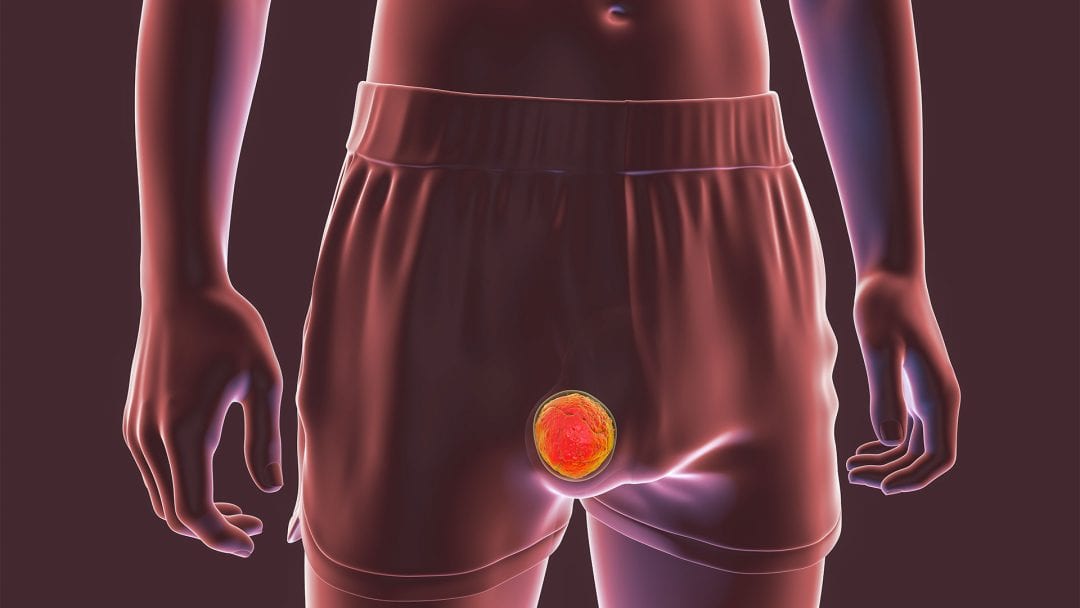
Testicular cancer mainly affects young men between the ages of 15 and 35 and becomes noticeable at an early stage of the disease. Symptoms can include swelling or hardening of the testicles, pain or a pulling sensation in the lower abdomen. Those affected often notice an obvious change in the size of the testicles.
Risk Factors for Testicular Cancer
Diagnosis and Treatment of Testicular Cancer
Diagnostics is based on physical examinations, imaging and biopsies. Early detection is crucial for successful treatment.
Conventional treatments for testicular cancer vary depending on the stage and may include removal of the testicle, radiotherapy and chemotherapy. In addition, the hormones produced by the testicles can be supplemented, which can prevent a testosterone deficiency.
Supportive measures from complementary medicine and naturopathy, such as the use of vitamin C, vitamin D or omega 3, can improve the success of therapy and minimize side effects. Hyperthermia and fever therapy have also proven to be effective methods for treating testicular cancer.
Dr. med. Karsten Ostermann M.A.
Advances in medicine have significantly improved cure rates, especially if the cancer is detected early.

Further information
The information listed contains relevant topics and serves to improve understanding.