Prostate Cancer
Prostate cancer is a common type of cancer that mainly affects older men. Prostate cancer often develops over many years without any noticeable symptoms. When symptoms do occur, they usually include: an increased urge to urinate, difficulty urinating, pain in the pelvic area and, in rare cases, bloody urine. From a diagnostic point of view, it is important to differentiate prostate cancer from possible prostatic hyperplasia and to initiate treatment at an early stage, while this can have a complete chance of recovery.
What is prostate cancer?
Prostate cancer, also known as prostate carcinoma, is a form of cancer that develops in the prostate, a small gland in the male reproductive system. The main function of the prostate is to produce the fluid for the sperm cells.
At just under 22%, prostate cancer is the most common cancer in men and is easily treatable if detected early. It occurs when cells in the prostate grow and divide uncontrollably. This excessive cell growth can lead to a malignant tumour that can expand and squeeze the structures in the urinary tract. In addition, prostate cancer can also metastasise to distant tissues and affect the entire body.
Age distribution of prostate cancer
Prostate cancer mainly occurs at an older age, from 50 onwards. While statistically, only one in 4800 men under the age of 35 is diagnosed with prostate cancer, this figure rises to one in fifteen among 75-year-olds. Regular screening should therefore take place with increasing age.
Nevertheless, even at a young age, if symptoms are present, a check-up should be carried out to rule out an aggressively growing tumour.
Symptoms of prostate cancer
Prostate cancer can often be asymptomatic in the early stages. However, if symptoms do occur, the following physical reactions may become noticeable:
Frequent urge to urinate: sufferers may experience an increased urge to urinate, which manifests itself particularly at night.
Difficulty urinating: Problems starting or stopping urination, weak urine stream or the feeling of not being able to empty the bladder completely.
Blood in the urine or ejaculate: The presence of blood in the urine (haematuria) or ejaculate may indicate prostate cancer.
Pain: Pain or discomfort in the pelvic area, lower back or thighs may occur.
Erection problems: Difficulty maintaining an erection can be a symptom of prostate cancer.
It is important to note that these symptoms can also indicate other diseases of the prostate or urogenital tract. You should definitely consult an experienced doctor for a more precise clarification.
Metastases in prostate cancer
Metastases in prostate cancer mean that the cancer has spread from the prostate to other parts of the body. The most common areas of the body to which prostate cancer can spread (metastasise) are the bones, particularly the spine, pelvic bones and thigh bones. However, other organs such as the lungs, liver or lymph nodes can also be affected by metastases from prostate cancer.
Metastasis usually occurs at a late stage. Therefore, it is very important to recognise the cancer early and remove the prostate. Once it has spread, it is almost impossible to cure it completely and the treatment is associated with significantly greater side effects.
Diagnosis of prostate cancer
When diagnosing prostate cancer, there are various methods that can ultimately support the diagnosis of prostate cancer. The digital rectal examination, determination of the PSA value, special blood values, ultrasound diagnostics and biopsy, are all part of the diagnostic measures for suspected prostate cancer.
Examination of the prostate
The digital rectal examination is a manual examination technique in which the prostate and rectum are palpated by the examiner in order to detect possible changes and hardening. If the urologist has the appropriate experience, the examination is reliable and therefore part of regular screening in old age.
PSA test
The PSA test analyses the prostate-specific antigen, which is produced by the prostate and can be elevated in the event of pathological changes to the prostate. We go into more detail about the PSA value below.
Blood values
The PSA value has been the golden standard in prostate examinations for years and provides information about changes in the prostate. The PSA value is elevated in cases of hyperplasia, inflammation and cancer and can support a suspected diagnosis in combination with other examination techniques.
In addition to the PSA value, alkaline phosphatase and LDH (lactate dehydrogenase) can be determined in the blood in order to recognise metastases in the bone.
Ultrasound
Ultrasound is a frequently used imaging method in the diagnosis and monitoring of prostate cancer. There are different types of ultrasound examinations that are used for prostate cancer:
Transrectal ultrasound (TRUS): this is a commonly performed method of examining the prostate. The doctor inserts a narrow ultrasound probe into the rectum. As the prostate lies directly in front of the rectum, the TRUS enables detailed visualisation of the prostate structure. The doctor can identify suspicious areas and, if necessary, take specific tissue samples (biopsies).
Transabdominal ultrasound: This method is performed through the abdominal wall (transabdominal) and allows a rough view of the prostate. It is less commonly used for the diagnosis of prostate cancer, but can be useful in certain situations such as monitoring the size of the prostate.
Doppler ultrasound: This special ultrasound mode measures the blood flow in the blood vessels. Doppler ultrasound can help to distinguish malignant tumours from benign ones, as cancerous tumours often have increased blood flow.
Biopsy
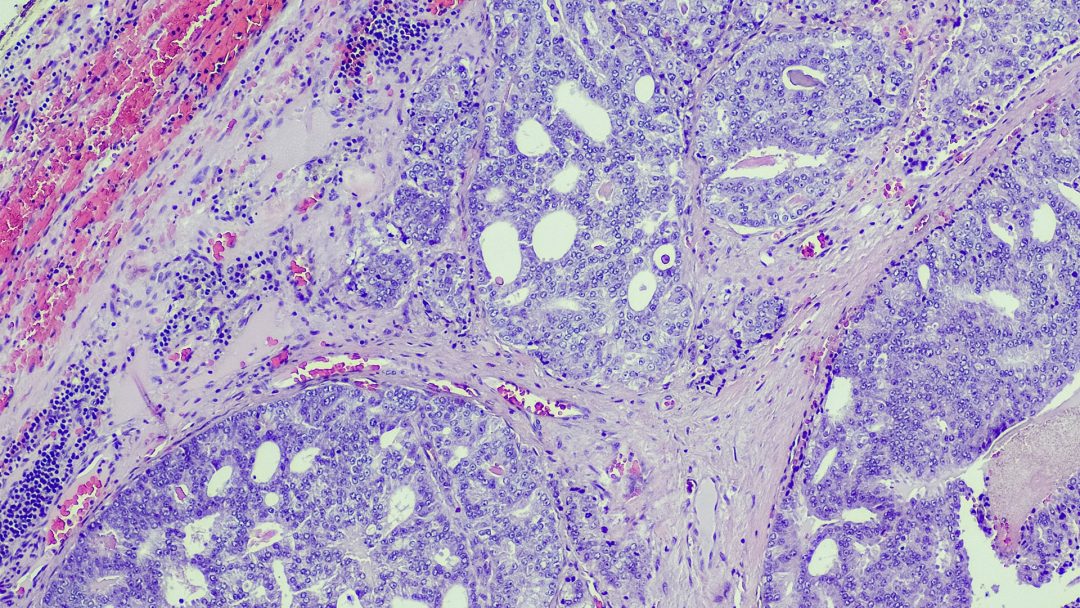
Biopsy plays a crucial role in the diagnosis of prostate cancer. Other diagnostic procedures, such as the PSA test (prostate-specific antigen), digital rectal examination (DRE) and imaging procedures can only provide a tentative diagnosis. However, only a biopsy can provide a definitive diagnosis.
After ultrasound-guided tissue sampling, the sample is sent to the laboratory and histologically analysed. Based on the exact visualisation of the cell types, a definitive diagnosis can be made in the laboratory.
PSA value
PSA, also known as prostate-specific antigen, is an antigen produced by the prostate. If the prostate becomes enlarged, inflamed or cancerous, the production of the antigen increases and the increased concentrations can be detected in the blood.
Especially in asymptomatic cases, the PSA status provides indications of possible diseases and is therefore an excellent basic screening tool.
Depending on age, there are different threshold values that can indicate a change. In addition, recurring determinations allow changes and their dynamics to be analysed very quickly so that treatment can be initiated at an early stage.
In addition, both free and bound PSA can be determined and the ratio of the two can provide information about the type of disease.
If the value is elevated, this is an indication for a biopsy to confirm the diagnosis.
Causes of prostate cancer
The exact causes of prostate cancer are not fully understood, but there are some factors that are associated with an increased risk of developing prostate cancer. It is important to note that the presence of these risk factors does not necessarily mean that a person will develop prostate cancer, and many men with prostate cancer have no obvious risk factors.
Conventional risk factors for prostate cancer include:
Age:
The risk of prostate cancer increases with age. The disease is more common in men over the age of 50, and the risk increases further with age.
Family predisposition:
Men who have had close relatives with prostate cancer may have an increased risk. A genetic link plays a role in this.
Ethnicity:
African-American men have a higher risk of prostate cancer than men of other ethnic groups.
Genetic changes:
Certain genetic changes or mutations can increase the risk of prostate cancer. However, this only affects a small number of cases.
Smoking:
Smoking is an additional factor that can increase the development of prostate cancer. In addition, the malignancy of prostate cancer is increased in people who smoke.
Increased toxin exposure:
Increased toxin exposure to various heavy metals, pesticides, herbicides and endocrine disruptors are suspected to be a possible cause of prostate cancer.
Treatments for prostate cancer
Depending on the stage and individual variations, there is a wide range of treatment options. The aim is to surgically remove the affected areas or the entire prostate or to destroy the cancer cells by radiotherapy before the cancer has spread.
If metastases have already developed, the aim is to slow down growth and contain further spread, as well as to ensure quality of life for as long as possible.
Conventional treatment
Brachytherapy
Brachytherapy is a form of radiotherapy in which the radiation source is introduced rectally in order to destroy degenerated tissue as precisely as possible.
This significantly reduces unwanted mutations in the surrounding healthy tissue.
Davinci prostate surgery
Surgery with a Da-Vinci surgical robot enables a minimally invasive, precise surgical result without large incisions and blood loss. The prostate, parts of the urethra and nearby lymph nodes are removed via small incisions in the abdominal wall, while particular attention is paid to the innervation of the sphincter muscle.
Cyberknife radiotherapy
Cyberknife is a form of radiotherapy in which the radiation source is introduced into the body and can act precisely. Healthy tissue in the surrounding area can be spared in this way.
Chemotherapy
Chemotherapy is mainly used for advanced, metastasised tumours. It does not act locally, but systemically, which means that the side effects are much more severe.
Hormone therapy
The administration of antiandrogens can block male sex hormones and inhibit the growth of prostate cancer.
Complementary medical treatment
Complementary medical treatments can support conventional therapies or represent an alternative if, after consultation with the oncologist, they are better suited to the individual case.
Hyperthermia and fever therapy
Measures such as hyperthermia or fever therapy can be used in prostate cancer and accelerate recovery.
Hyperthermia in the treatment of prostate cancer
Combined hyperthermia and radiotherapy for prostate cancer: a systematic review
Hyperthermia and Radiotherapy in the Management of Prostate Cancer
Current Role and Future Perspectives of Hyperthermia for Prostate Cancer Treatment
Mistletoe Therapy
Mistletoe therapy is also promising for prostate cancer.
Boie D (1977). The additional Helixor therapy in stage D prostate carcinoma. Report. Rosenfeld, Association for Leukaemia and Cancer Therapy.
Chances of cure for prostate cancer
The chances of a cure for prostate cancer are very good, especially if it is detected early. Nevertheless, there are many factors that significantly influence the success of the treatment.
These include the aggressiveness of the tumour, the stage or progression of the disease and possible metastases. Furthermore, the chance of recovery is significantly influenced by the general state of health and the chosen treatment method.
If the cancer is diagnosed in the early stages, the 5-year survival rate is around 90%.
Home remedies for prostate cancer
It is important to note that home remedies alone are not enough to treat prostate cancer. Prostate cancer requires professional medical care and appropriate treatment.
However, there are lifestyle factors that can help promote overall wellness and reduce the risk of prostate cancer. For example, a healthy diet rich in antioxidants and high-quality fats forms an important basis. Avoiding smoking and regular exercise are also basic requirements.
Lycopene
Many studies suggest that the active ingredient lycopene, which is found in tomatoes and hawthorns, for example, can slow down the growth of prostate cancer. Lycopene can also be taken in the form of a high-quality dietary supplement. Clarification and constant monitoring by an experienced doctor are highly recommended.
Lycopene exerts anti-inflammatory effect to inhibit prostate cancer progression
Green tea
Drinking green tea is also recommended for prostate cancer and various studies confirm its supportive effect. Here too, a doctor should always be consulted in order to initiate and monitor the correct therapy.
Anti-Cancer Effects of Green Tea Polyphenols Against Prostate Cancer
Effects of Green Tea Catechins on Prostate Cancer Chemoprevention: The Role of the Gut Microbiome
Green tea polyphenols for prostate cancer chemoprevention: A translational perspective
Green tea extract for prevention of prostate cancer progression in patients on active surveillance
Pomegranates
Studies have also shown that pomegranates can have a supportive effect on prostate cancer. A targeted intake should also be clarified by a doctor in order to avoid imbalances, intestinal complaints or intolerances.
A review of pomegranate in prostate cancer
Pomegranate and its components as alternative treatment for prostate cancer
Prevention of prostate cancer
The aim of prostate cancer screening is to detect the cancer at an early stage so that it can be treated as effectively as possible and its development prevented.
This includes a digital rectal examination and PSA determination, a sensible risk assessment in the presence of risk factors, a healthy diet and an active lifestyle.
If risk factors such as a family history are known, it is advisable to talk to your GP to clarify individualised prevention options.
Even though a large proportion of developing cancers are due to genetic causes, it is important to understand how our lifestyle influences diseases and even our epigenetics. Therefore, leading a healthy lifestyle and minimising known risk factors should always be a top priority.
Life expectancy with prostate cancer
As already mentioned, life expectancy with prostate cancer is very high. The 5-year survival rate for treatment in the early stages is 90% and even with advanced metastasis, life expectancy can still be years. However, this is only possible with appropriate treatment and compliance on the part of the patient.
It is not only the pure life expectancy that is important, but also the quality of the remaining life. As requirements and wishes are very individual, treatment must always be customised accordingly.
For example, chemotherapy can be the right approach for many patients, while others do not want to accept the associated side effects and consciously decide against it.
Psychotherapy can also help to make the remaining time of life more pleasant. If you need help, you should communicate this openly with your doctor so that support can be organised promptly.
Prostate removed, what is important to know?
As with all cancers, regular screening is an important part of aftercare. In 30% of those treated, tumours recur and need to be treated again.
You should also be aware of the possible side effects of removal. Unfortunately, impotence and incontinence are difficult to avoid, as a central nerve plexus is attached to the prostate and can be damaged during the operation.
Possible impotence after prostate surgery
Even with modern surgical techniques, it is not always possible to avoid damaging the sensitive nerve plexus. Impotence occurs in 20 – 80% of cases (statistics vary widely), which can severely impair quality of life.
If you have any worries or concerns, you should talk to your doctor about possible solutions.
In some cases, the problem improves after several months; in others, medication or implantation of prostheses can provide relief.
Possible incontinence after prostate surgery
For many patients, the risk of incontinence in particular is a major obstacle to deciding in favour of surgery. The symptoms usually improve within a few months. However, possible incontinence after prostate surgery can also persist in the long term and thus lead to a high level of suffering for those affected.
Changes in the ejaculate
It is also important to be aware of changes in the ejaculate before the operation. Most men are unable to conceive after radical prostatectomy. Sperm freezing is a possible option.
Med. pract. Dana Hreus M.A.
Treatment of prostate cancer can have a higher success rate if experts from different medical fields work together and take an integrative approach to patient care.

Frequently asked questions and answers about prostate cancer
The topic of prostate cancer and prevention raises many questions for affected patients. The most frequently asked questions are answered below.
If you have any further questions, please do not hesitate to consult your doctor.
The average age at which prostate cancer is diagnosed is typically around 65. However, it is important to note that prostate cancer can affect men at different ages.
The risk increases with age, and the majority of cases occur in men over 50.
It is advisable that men talk to their doctor about their personal risks and the appropriate screening to detect and treat prostate cancer in time.
To detect prostate cancer at an early stage, every man over the age of 50 with health insurance in Switzerland can have a palpation examination of the prostate and a PSA test every two years.
If you have existing risk factors, early screening can be useful. Consult your doctor about this.
Some studies have suggested that regular consumption of pomegranate juice may be associated with a slower progression of prostate cancer. Nevertheless, consumption is by no means a substitute for proven screening and treatment methods and should always be discussed with your doctor.
It is thought that lycopene could have a protective effect due to its antioxidant properties and its possible ability to have an anti-inflammatory effect. Consequently, a diet rich in red fruits such as tomatoes, rosehips, watermelon and pink grapefruit may be able to slightly reduce the risk of prostate cancer. Consultation with an experienced doctor is recommended.
As prostate cancer cells react to high testosterone levels with growth, testosterone therapy can lead to a rapid progression of prostate cancer. If hormone treatment is already in place, screening should therefore be started earlier in order to be able to intervene at an early stage.
Incidental prostate cancer refers to a chance finding of prostate cancer during a diagnostic examination or operation that was not originally performed to diagnose cancer.
Yes, there are benign prostate tumours, which are known as prostate adenomas or benign prostatic hyperplasia. They can also cause health problems.
Further information
The information listed contains relevant topics and serves to improve understanding.