Chronic Obstructive Pulmonary Disease (COPD)
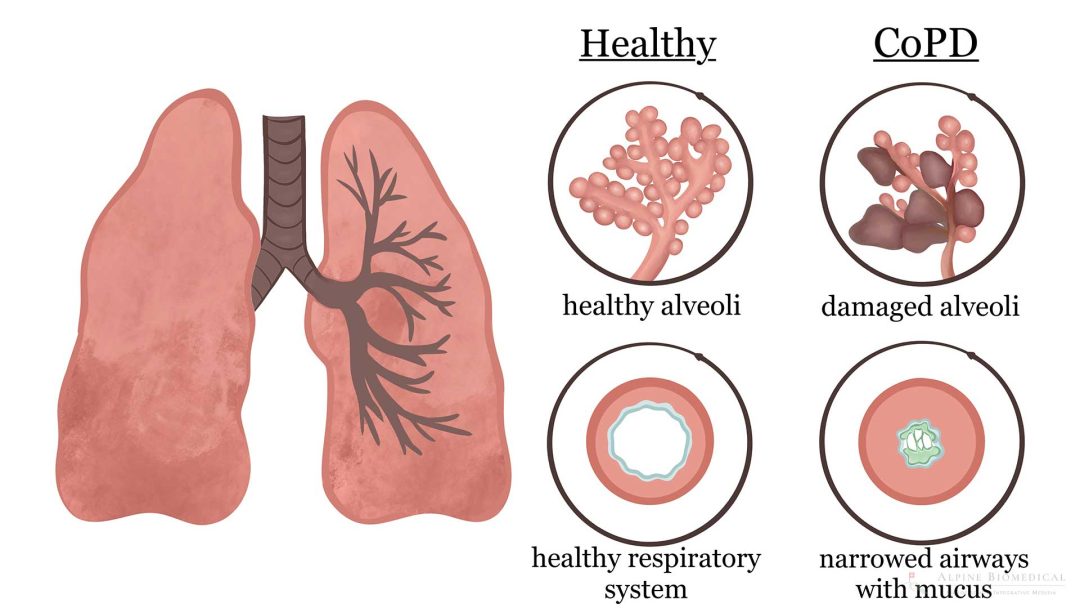
Chronic obstructive pulmonary disease (COPD), also called smoker’s cough, emphysema or chronic bronchitis, is a common lung disease causing restricted airflow and breathing problems. This narrowing of the airways is due to a permanent inflammation and swelling of the bronchial mucosa. Moreover, the lungs are clogged with phlegm. Prevention consists of avoiding the main causes, which is the inhalation of harmful substances such as smoking. The damage is irreversible and incurable, but treatments can improve the quality of life.
Dr. med. Karsten Ostermann M.A.
An integrative health approach with different specialities can help prevent COPD and improve the quality of life when the disease progresses.

Further information
The information listed contains relevant topics and serves to improve understanding.